Corona Science Journal
Note: I have been unable to keep up with the latest developments as I have shifted my efforts to a Dutch-language daily blog about positive COVID-19 developments, while keeping it real. You can read it here. Google Translate does a surprisingly good job on this.
There is sufficient other content out there that aims to tell you if things will be bad or not. A lot of data can be found in Coronavirus Primer for Reasonably Rational People.
I have no specific epidemiological expertise, so I won’t add to these existing efforts.
What I can do very well however is read statistics and papers and determine if some trend or conclusion is forming. There are enough big questions out there that don’t get the attention they deserve. Sadly there is also a lot of bad information and even some (very) bad science going round. In this document I try to filter out the stuff which has a consensus forming around it, or looks very plausible.
Here goes.
Feedback, content & interesting links are VERY welcome on bert@hubertnet.nl or @bert_hu_bert. Many readers are sending me a steady stream of updates, please keep it up! Special mention for Oliver Germer who appears to be combing the internet for the best data.
Notes
I have removed links to the French hydroxychloroquine work. Drug might still work, but we can’t tell based on that data.
Summary
For regular readers, here is a summary of the latest (30th of March) picture, details are in the rest of the page:
- All evidence continues to point at COVID-19 being a normal virus to which people develop immunity (but likely not lifelong).
- It appears there is now a reliable way to test if someone has developed COVID-19 antibodies. This will tell us in a 10-minute test if someone is now likely immune. Update: many actual tests appear not to be reliable.
- Several medicines have now seen encouraging small scale initial trials. These trials have strong limitations, but if I read the tea leaves right, it seems likely that at least a few of these things will pan out. There is sufficient smoke to suggest a fire. But despite what Trump says, we are very much not out of the woods yet.
- Many countries have now shown it is possible to suppress local COVID-19 transmission, if a country/society/government works hard enough on it, but everyone has to do the work of physical distancing, testing, isolating and treating.
- Many vaccines are in development or even earliest forms of testing, but none of the fast trajectories have a strong track record of protecting human beings.
- A veritable TORRENT OF SCIENCE is happening. In this link every relevant paper is briefly annotated, and there are frequent updates.
Facts
Most things COVID-19 are not yet facts because everything is so new. Here is a brief collection of things we do know for sure:
- It is far, far worse than seasonal flu. Anyone who doubts this should look at the photos and videos from Wuhan and Northern Italy, or the graph below.
- Younger and healthy people may do fine (’not die a lot’), but many people are not young or healthy, and we care about them too.
- Slowing down the pandemic makes sense since it buys time for our healthcare systems and scientists to learn. It also spreads “peak illness” so our systems get less overloaded.
- Washing hands with normal soap, coughing hygiene, and “social distancing” are very effective in limiting the spread. Social distancing means not going to that party and not organizing that event, and likely eventually not going to work or school.
The first feedback I got on this page was “it is just like the flu”. This graph from South Korea, where hundreds of thousands of tests have been performed, shows the difference:
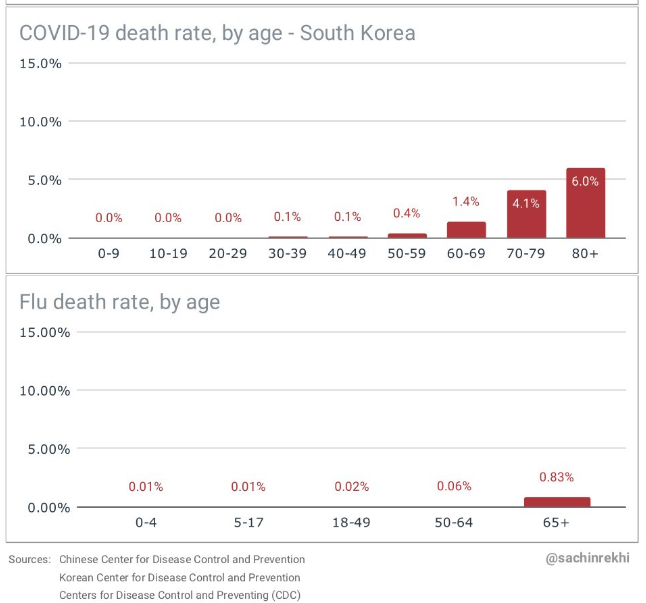
Note that because of the hundreds of thousands of tests in South Korea, they have also captured tons of asymptomatic people and not just hospital cases.
This article Coronavirus: Why You Must Act Now is also very helpful.
Will summer/warmer weather help?
The official WHO word on this is “there is no evidence, don’t count on it”. Hope is not a strategy, and warmer weather in the northern hemisphere will do nothing for the south, but it remains a pertinent question.
One may wonder if the pretty low numbers from warmer and more humid countries are fake (perhaps outright faked, or just not doing testing), but they will eventually tell us a story.
The countries to watch are those that are less organized or have less resources to fight an epidemic, but are currently having hot and humid weather, without universal air conditioning. Large outbreaks are very hard to hide, and can even be seen from space. An absence of such a large outbreak would be a strong data point that warmer weather might help.
Watching this one closely. There are papers that argue either side (it will help/it won’t help). Note that “help” does not need to mean it kills the virus - in our goal to stem the epidemic, even 10% reduction in transmission can be helpful if it takes the reproduction number just under 1.0.
Some discussion is in this AP article on Snopes.com (!).
The inestimable Marc Lipsitch has also weighed in: Seasonality of SARS-CoV-2: Will COVID-19 go away on its own in warmer weather?: tl;dr: probably not.
Update 30th of March: If I speculate a bit (beware!), I personally think that we can see that warmer more humid countries are having a slightly easier time. This is congruent with the reproduction number being somewhat depressed there, even without further measures. Still means strong measures are necessary, but they may be more effective. Speculation ends.
Masks
Previously noted at the very end of this page:
- The Mask Question: all of Asia believes in wearing masks, the rest of the world tells us to leave the masks to professionals. What is it? Zeynep Tufekci weighs in here. Meanwhile the Cochrane review has the following
Based on 34 papers, it is now starting to look like:
- Best way not to spread COVID-19 is not to be close to people. No mask is better than this. Full stop.
- If you have to go out and can’t avoid it, almost anything covering your
nose and mouth will reduce the rate at which you spread the virus, should
you have it.
- You won’t know you have it for the first few days, but you can still spread it. Many many COVID-19 patients are completely asymptomatic, but still spread the virus. So assume you are infected.
- You don’t need a medical mask to achieve a good effect
- Very moderate evidence if a mask might protect you individually.
The above seems to be uncontroversial, but it flies in the face of previous non-Asian government messaging. Czechia and Austria now recommend masks.
The public health story is also very difficult. If people assume a mask protects them, they might start going out more, possibly defeating the effect of reduced transmission.
Very clear messaging will be required.
Risk factors
Many statistics are now available on who is dying or being ventilated, but not many clear things are emerging beyond “try not to be old”. There is a lot of noise too. Many old people are hypertensive, many old people are overweight/obese, we need better statistics to try to filter out if there are signals in there.
One relatively clear signal appears to be that smokers are at a far greater risk. The data is not that strong yet, but now is a great time to stop smoking. Now is also a great time not to take more risk because you are not a smoker, since the data is not that strong.
Interesting trials
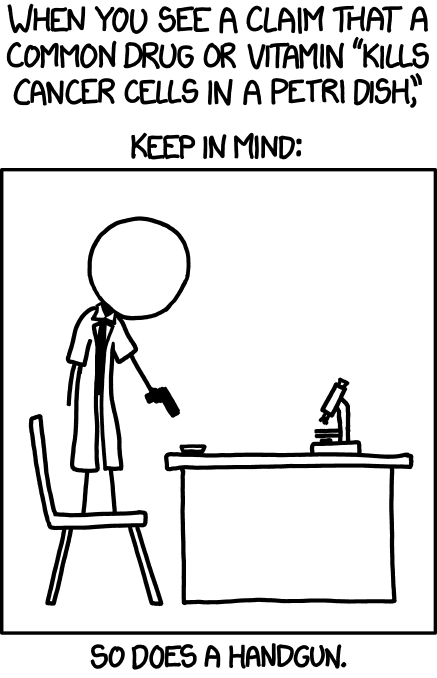
Many trials are currently happening or being launched. Running a good trial is very difficult and it is easy to expend great effort and come up with unreliable results. As an example, since the vast majority of people recover from COVID-19, you could do provide a group of patients with (say) Dutch cheese, wait two weeks, and conclude that 85% recovered. Yay for Dutch cheese!
Even with a control group (that gets fake Cheese) it there are lots of ways to fool yourself into thinking you got a result, especially when we are looking for non-dramatic effects. For example, a treatment that shortens ICU stay by 20% is exceptionally useful, but 20% needs to be picked up out of the noise.
Another terrible way to ruin your study is to run it, look at the disappointing results, and then recast your hypothesis. For example, medicine X might be so-so effective, but a subgroup that got X and Y all survived. Statistics teaches us that it is folly to now announce X+Y are a cure, until you rerun a trial where you pre-determine that X+Y is what you are testing, or perform extensive Bonferonni-correction on your statistics.
Smaller trials are also not very sensitive and could more easily be wrong, or not be “powered” enough to see important effects like when a drug only works when it is provided early enough.
Having said all this, here are some properly designed trials (or campaigns) that are interesting:
- The big one: the WHO SOLIDARITY trial launched in response to several smaller and inconclusive smaller initiatives. As noted in this excellent STAT article this trial will test remdesivir; a combination of two HIV drugs, lopinavir and ritonavir; lopinavir and ritonavir plus interferon beta; and the antimalarial drug chloroquine. The trial design is interesting and 10 countries have already signed up.
- BCG vaccination against TBC. This sounds odd but it has been long noted that the BCG vaccination temporarily boosts the immune system in general. Two Dutch universities had long been investigating this phenomenon, and has now obtained emergency permission to test the hypothesis on 1000 hospital workers, 500 of whom will be the control group. Goal is to see if this leads to fewer infections.
- The Dutch blood banks are now screening all donations for a week for presence of COVID-19 antibodies. They go through 10k donors/week, out of 331k registered blood donors. This will give a sensitive indication on the amount of established immunity in the population. Some brief news in English, will add more detail as I find it.
- Ongoing for a few days already, a trial to test if chloroquine provided quickly after potential exposure might be protective. This one is very exciting since it offers a potential strategy that could prevent significant harm.
- An overview up to date until the 20th of March is here
Please contact me is you know of more interesting trials - I mostly pick up local ones on my own.
Testing, infectiveness
Earlier I wrote a bit on how COVID-19 testing works, it is important to realise that this is effectively “searching for viral genetic material in swabs”.
While it is amazing how this works, it does come with limitations: a swab in the wrong place might miss the virus. And the other way around, just because viral RNA is present, this does not have to come from competent virus particles that can infect people.
This recent paper “Clinical presentation and virological assessment of hospitalized cases of coronavirus disease 2019 in a travel-associated transmission cluster” discusses the nuances. This statnews.com article provides a good explainer, and I recommend that you read it. But two key sentences “Importantly, the scientists could not grow viruses from throat swabs or sputum specimens after day 8 of illness from people who had mild infections.”, but also “The researchers found very high levels of virus emitted from the throat of patients from the earliest point in their illness —when people are generally still going about their daily routines. Viral shedding dropped after day 5 in all but two of the patients, who had more serious illness. The two, who developed early signs of pneumonia, continued to shed high levels of virus from the throat until about day 10 or 11.”.
Another way of testing is by measuring if a patient has generated antibodies against COVID-19. This is a fascinating area which I am reading up on (books have arrived). There are early and later antibody responses (IgM and IgG respectively). Excitingly, it appears to be possible to determine presence of IgM and IgG for COVID-19 in 10 minutes based on a drop of blood. Less excitingly, it also appears IgM is only present 1 or 2 weeks after infection (or perhaps 3-5 days according to another commercial source.
One such test is described on this page, which includes manuals and protocols.
Note: I wrote a separate warning about buying these tests online. Please feel free to forward this warning to people considering buying a rapid at home “self-test”!
It appears that such a test will mainly allow you to ’look into the past’ - even if someone recovered, I think you can still see IgG antibodies.
This kind of testing may have a role, but it is no substitute for doing PCR, which takes hours, requires special equipment and is quite laborious, but can detect the disease at an early stage.
18th of March update: The paper “A serological assay to detect SARS-CoV-2 seroconversion in humans” notes that at least one test is specific and sensitive and picks up IgM as early as 3 days post symptom onset. This is great news.
A brief intermezzo: reading about medical breakthroughs
Because I keep track of a few unfortunate medical conditions for family and friends, I am quite well versed in reading about “medical breakthroughs”. These happen a lot, at least on paper. It takes quite some skill to find out if there is an actual breakthrough behind the hype.
I wrote about this before way back in 2013, but in short, we have a veritable chain of people who “want to believe”, including us. This can distort the reality.
A cautious observation during patient treatment (‘14 out of 20 patients improved in clinical measurements’) is spiced up slightly by the institute PR department to ‘most patients improved’. A journalist, who also wants to believe may spice this up a bit more: ‘most of the patients tested were cured’. Meanwhile, we as readers also want to believe, so we might not pay that much attention to caveats. For example, perhaps the “cure” worked, but only on a very specific subclass of patients. If we don’t pay real close attention, we may end up believing we read there was a cure for the whole disease.
Keep this in mind when reading about COVID-19 cures or treatments that will surely be reported in the coming weeks.
Specific things to look out for:
- You read about the news on a site you’ve never heard of before, or, it is on a known site full of nonsense like the Daily Mail. Note that even ‘big name publications’ fall for sensational news.
- There is no way to find the actual research (this could be names you can Google, institutions or best, links to an actual preprint or paper)
- The news is only about a few cases in a single hospital
From what I see, in the coming days/weeks we will be seeing some actually encouraging news, but we’ll be seeing way more nonsense. So be careful!
Antiviral medicines: will they help?
This is actually a more complicated question: who will they help and when? Many anti-virals actually perform as promised, and inhibit viral replication both in the lab (‘vitro’) and in primates or even people (‘in vivo’). But many papers note that best effects are achieved when the medicine is dosed either slightly before (!!) infection, or shortly after.
This may be very helpful to stem an outbreak (if the medicine is widely available, easy to administer and safe), but it is not necessarily much use for someone already in the intensive care unit.
Trials of various anti-virals are proceeding, some encouraging hints have been picked up here and there, but there is no solid data yet.
The big ones to watch are Remdesivir and (Hydroxy)Chloroquine (an older Malaria medicine, but with side effects and contra-indications), with an honerable mention for Camostat, which is already approved in Japan for other treatments.
It appears hydroxychloroquine is 5 times more effective in vitro but many national treatment plans (like the Dutch one) default to chloroquine since it is better known. I hope hydroxychloroquine will also be tried!
Note that despite Donald Trump’s enthusiasm, we still have no data on the actual effectiveness of ‘hclq’ or ‘clq’ in treatment. Some of the data coming from France is highly suspect, so it can’t be relied on. That does not mean the drug is not effective however - we still just don’t know. There are plausible reasons why ‘hclq + zinc’ might work, for example.
20th of March update: A thread by the incomparable @DGlaucomflecken on the effects on eye-sight for short term treatment can be found here. In short: this should not be a problem.
Some slight optimism on Remdesivir can be found in this Guardian article which notes that the producer has ramped up production in advance of the outcome of trials (10th of March). A further positive third-hand anecdote can be found in this tweet, which notes it even works on gravely ill patients, and even without completing the 10 day course. But it is a third-hand anecdote, and it notes doses are scarce.
This is PURE speculation, but we might get lucky that specifically hydroxychloroquine might be effective early in the disease and that we can send it out to everyone who even appears to be infected. We don’t yet have data on if this would work, but it is reasonably plausible. Anecdotal tweet.
17th of March Update: there is now a clinical trial of this idea so at least I am not alone in speculating.
17th of March third update, a trial of favipiravir has finished in China, with some encouraging results: The results have shown patients treated with favipiravir took four days before being tested negative, whereas the control group took 11 days.. This is a press report and not a preprint. 19th of March, some further press in The Guardian.
Could some medicines be making COVID-19 worse?
Pure speculation: Hypertension is a major major risk factor for dying from COVID-19. COVID-19 uses the ACE2 receptor for entry into cells. Common high blood pressure medications increase expression of ACE2 mRNA. Here is some speculation in a BMJ response letter on if these medicines could possibly make things worse for users. Very speculative. A great summary of the situation: The Coronavirus Conundrum: ACE2 and Hypertension Edition.
Heart and bloodpressure professional bodies have been swift in stating there is nothing wrong with the existing medications (from the ‘Coronavirus Conundrum’).
Meanwhile the incomparable MD Malcolm Kendrick (I’m biased, he’s one of my heroes) has weighed in. By parsing Italian statistics he has derived it is likely >52% of COVID-19 deceased patients were on either ACE inhibitors or ARB therapy.
Through further reasonable assumptions, he derives that only 14% of the general older population in Italy are likely taking these two drug classes.
This does appear to be rather strong data point although it would be wonderful if we also had numbers on alternate hypertension medicines.
Supportive medicine
This is pretty new stuff, perhaps too new to report on yet, but it does look interesting. Immune systems can beat the virus, but you do have to stay alive while they do it, and this is actually what hospital and intensive care units are trying to achieve.
There are early reports that Tocilizumab / Actemra has been effective on patients in Italy and China. But these are very early observational reports. Actemra is a ‘blockbuster’ arthritis drug, so we know a lot about it. As of the 11th of March, there are a mounting number of anecdotes that Actemra is effective for certain patients, and Italy is rolling out broader use. There is now also a Lancet paper.
17th of March update, Italy is launching a 330-patient Tocilizumab trial after some further positive experiences in several hospitals.
21st of Match update, Roche is launching a clinical trial in April.
In short, these medicines do not specifically kill or inhibit the virus, but they aim to help fight off its effects & keep the patient alive.
Monoclonal antibodies
This is extremely fresh. A collaboration between universities in The Netherlands (Erasmus and Utrecht) has developed a monoclonal antibody that binds to the COVID-19 virus, and in doing so disrupts its proliferation. This is based on previous research on SARSv1, so they had ’everything ready to go’. Details are in “A human monoclonal 1 antibody blocking SARS-CoV-2 infection”. Note that this was an international paper by lead authors Chunyan Wang, Wentao Li and Dubravka Drabek.
Monoclonal antibodies (‘mabs’) are still relatively recent, but some of them have been spectacularly effective. And expensive.
This specific antibody with the exciting name 47D11 appears to bind very well to both SARSv1 and COVID-19. At the very least this might enable fast and simple detection of an infection, since it binds directly to the virus, without having to do all kinds of RNA and DNA processing.
With some further luck, 47D11 might also be of clinical use. I am very far from an expert, but the concentrations at which this new ‘mab’ is active appear to be feasible, requiring milligrams per patient if I read it right.
This last bit is relevant - by now we all know lowly soap also eviscerates COVID-19, but the problem is that at concentration required, it would also kill us. Turns out our bodies use lipid bilayers as well.
Will 47D11 be useful on the timescales we need? I don’t know. Some background can be found in this interview.
Convalescent sera: using blood from recovered patients
Patients that have recovered will have generated COVID-19 specific antibodies. These can be used to help cure current patients, or to temporarily protect non-infected people, for example key medical staff.
Convalescent sera have a storied history of working and sometimes not, a great discussion can be found in The convalescent sera option for containing COVID-19, which notes that it likely works best for very recently infected patients, or early in the course of the disease.
Vaccines
To be honest I have little clue. There is frantic ongoing activity by dozens of groups and companies. The WHO lists 41 (or 42) active efforts. We don’t currently know if any of these vaccines will work (safely), nor how quickly they can be produced if they do. Also, who would get them? Countries turn very nasty over such things.
Some good discussion on vaccines and other treatments can be found in this Science article.
This situation will hopefully clear up over time. It may be that small quantities of vaccines become available early and could be used in targeted fashion.
It may also be that nothing works. But, a lot of attempts are being made and there is solid science behind the efforts. According to this informed Twitter thread by someone that wrote a book about it, we have managed to create veterinary vaccines for several corona viruses, there just never has been a need to do so for humans. But it shows it can be done.
Meanwhile, it appears one German company CureVac, which makes mRNA-based vaccines, is being enticed to work for the US exclusively. Perhaps they know something we don’t. This story is very messy. CureVac has previously used their technology to make what appears to be a functioning rabies vaccine.
A brief word on mRNA-based vaccines. For an DNA/RNA primer, try my earlier post ‘What is life’ or the followup ‘Is biology too complex to ever understand?’.
So in short, our cells convert (’transcribe’) DNA from our genome into “messenger RNA”. Messenger RNA (mRNA) is subsequently converted (’translated’) into proteins. When a virus infects a cell, it hijacks this mechanism by also creating mRNA, and turning the cell into a factory for new viruses.
What an mRNA-based vaccine attempts to do is to get carefully crafted mRNA inside our cells so those cells start producing proteins we have chosen. We pick proteins that also occur in (or on) the virus we want to generate immunity for.
If done well, those cells will create those viral proteins, and our immune system will get alerted to these alien proteins and develop antibodies and hopefully long-lived immunity.
The nice thing about this trick is that the mRNA in an mRNA-vaccine does not self replicate. So if you inject x amount of vaccine, at most y amount of protein will come out. And you can calibrate y that it won’t actually kill or harm the patient.
In a sense, an mRNA-vaccine is sort of a ‘build it yourself’ vaccine that uses our own cells to create proteins that look like viral proteins (or actually are), and then our immune system does the rest. IKEA-style vaccines if you will.
There are also self-amplifying mRNA vaccines that do replicate and multiply in our cells, which leads to a more potent immune system response, but is in a sense playing with fire.
mRNA-vaccine technology is pretty well advanced and has conquered many hurdles already, but has as yet not delivered any vaccine against a Corona or Influenza virus in humans. It has done so in mice however. A very good writeup is in this Nature article, which is the source of most of this section.
Of note, some pretty clever things are already in the works to stimulate the immune system to act on the newly generated viral proteins. If I had to guess, it looks like the field is maturing rapidly and it all does seem plausible. But there’s no proof in humans.
One final thing mRNA vaccines have going for them is that they can be produced quickly. So let’s see if this delivers.
Can you stop the epidemic?
Oddly enough, it does appear you can pause it with great effort. Notably China, Hong Kong, Singapore, Taiwan appear to have been able to slow down things hugely. Various academic papers have derived that after measures were in place, every patient infected only 0.3 new patients in Wuhan. But with a drastic impact.
It is still early but the numbers coming out of South Korea are definitely improving. South Korea notably did not completely shut down its country in the way Wuhan is still (9th of March) locked up.
So it appears that if a country (government AND its people) really wants to and has the means, it can slow down the spread hugely.
An open question is if you can do this and remain a long-term viable economy. Also you have to want it, and many countries appear to wait with measures until they are unavoidable. This will not be of any use. The right time for measures is when they appear to be overreactions - they will be visionary soon enough.
Actual treatment guidelines
One of the reasons it makes sense to try to slow the epidemic is that it buys time to learn about treatments.
Some governments are publishing their guidelines, sometimes even in English:
- Chinese treatment guidelines as translated by China Law Translate (thanks!)
- Dutch treatment guidelines - in Dutch, but quite thorough. Updated every few days.
- Belgian guidelines, in English!
- Italian guidelines, in Italian.
- UK guidelines
The Chinese guidelines briefly discuss Tocilizumab.
This Google Document containst a list of treatment guidelines, also from Korea. I touches a lot on (hydroxy)chloroquine as well.
(more links welcome!)
Is this a normal virus? Can you get reinfected?
Everything points towards COVID-19 being a normal virus that generates a normal immune response, which should provide protection against reinfection, at least in the short term.
There are some (two, that I know) reports of reinfection, but they are very sparse so far, and one is thought to be a testing mishap. An experiment in rhesus macaques showed they could not be reinfected (after a month). This is great news if you are a rhesus macaque, but it likely extends to humans as well.
It is however unknown how long built up immunity will last, and also how strong the immune response remains. A weaker response might turn an infection into a far less dangerous but still inconvenient affair. We know surprisingly little about this. There is a paper on coronaviruses IN MICE, which indicates a robust response at least for one year. Update 17th of March: here is an extremely thorough paper on the very normal immune system response to even mild COVID-19 disease.
Update 19th of March, here is a 1990 paper The time course of the immune response to experimental coronavirus infection of man that shows that after a year, antibodies for a coronavirus can still be detected, but at low levels, but that on re-exposure, patients technically get infected (briefly), but do not actually get ill.
Although (rapid) reinfection currently does not appear to be a big thing it is of course a subject of intense interest, so this paragraph will be updates with everything we learn.
What about Ibuprofen/NSAIDs?
Here is what I understand is the full list of things we know about the safety of Ibuprofen during pneumonia:
- …
The warning to not use Ibuprofen from the French minister of health (who is also a doctor) came without evidence or data but it also did not come out of nowhere.
People frequently refer to a paper in The Lancet, but it only mentions Ibuprofen in passing, without adding data.
In the absence of real data, it appears that if you have the choice between Ibuprofen/NSAIDs or paracetamol (tylenol, acetominophen), use the latter, a recommendation echoed by the WHO, and also by this BMJ article. 19th of March update, WHO is no longer sure but does confirm there is no data.
There are some unfortunate health authorities, including Dutch ones, rubbishing the Ibuprofen warnings - I can’t see how they do this since there is an utter lack of data showing NSAIDs are safe or beneficial in these situations. Best response right now is “we need more data, but it could well be true”.
Will update this section as more data becomes available.
Can we restart society after lockdown? (beware, speculation)
The rest of this page is purely based on well reported science and serious sources. In this section I speculate a bit. Please be aware of the difference, this is me thinking out loud, and I am no expert.
From personal sources, I am convinced China is indeed starting up its economy again. Even some Hubei (the Wuhan province) based companies where I have second hand contacts are shipping things again to people I know.
It is estimated that around 1% of Wuhan got infected at peak. This is very very far away from any kind of “herd immunity”. Other sources say 4%, but this is still not a lot.
So how is it possible things are starting up there again without the virus roaring back? And similarly, how come other large cities there did not get huge outbreaks even with far more relaxed measures?
I think we are missing some factor. If I do some non-expert speculation (sorry), many cases of COVID-19 may have been PCR-negative (so never detected), but perhaps did lead to some kind of immunity. Serological testing (the IgG, IgM story from above) will likely tell, and I anxiously await the results.
It may also be that COVID-19 depends to a far larger extent on ‘super spreading events’ and simply not doing very large gatherings is all you need to keep things under control. Who knows.
Or perhaps extreme contact tracing for each remaining event is enough to keep things under wraps once the explosive phase is over.
Could it be that masks do help if worn by all people that might be infected?
Perhaps it is a combination of multiple factors that, after the initial outbreak is under control, drives down the reproduction number under 1 without halting your whole society. A combination then of some immunity, less super spreading, masks, more favourable weather, perhaps.
Some thoughts can also be found in this interview with Nobel-prize winning biophysicist Michael Levitt who called the peak of infections in Wuhan correctly.
Marcel Salathé, a professor of digital epidemiology, describes a post-infection peak scenario in this post where he estimates that once the worst is past, stringent and high-capacity testing followed by isolation will keep things under control. Perhaps that is what we are seeing.
Meanwhile, Marc Lipsitch who is an expert (linked below from the Twitter section), opines that Wuhan didn’t solve anything and that if they relax their measures, the virus will just come back.
In “Strongly heterogeneous transmission of COVID-19 in mainland China: local and regional variation” we can read an analysis that indicates that outside of Wuhan, after people were warned, the reproduction number of COVID-19 was below 2, even before strong measures were implemented. This may also explain some of the relative ease of keeping things under control in China, but unsure.
There is a good and informed 19th of Match Twitter thread by Trevor Bedford (a scientist who studies viruses, evolution and immunity) on keeping society running with COVID-19.
Wild speculation ends here!
Graphs and numbers
There are so many graphs and numbers out there. Please be aware that we have no ‘Corona-meter’. All the numbers and especially the graphs we see are the product of many policity decisions of whom and how many to test. Some tests may also be more sensitive than others. Almost no country reports reliable numbers on who is cured. We may ache for the certainty of hard figures, but the numbers just don’t work that way.
One site that does appear to be making an effort is “Temporal variation in transmission during the COVID-19 outbreak” by the UK’s Centre for Mathematical Modelling of Infections Diseases.
By comparing numbers not among countries but comparing them from day to day, they can derive growth factors. They also attempt to account for the delay in reporting new cases.
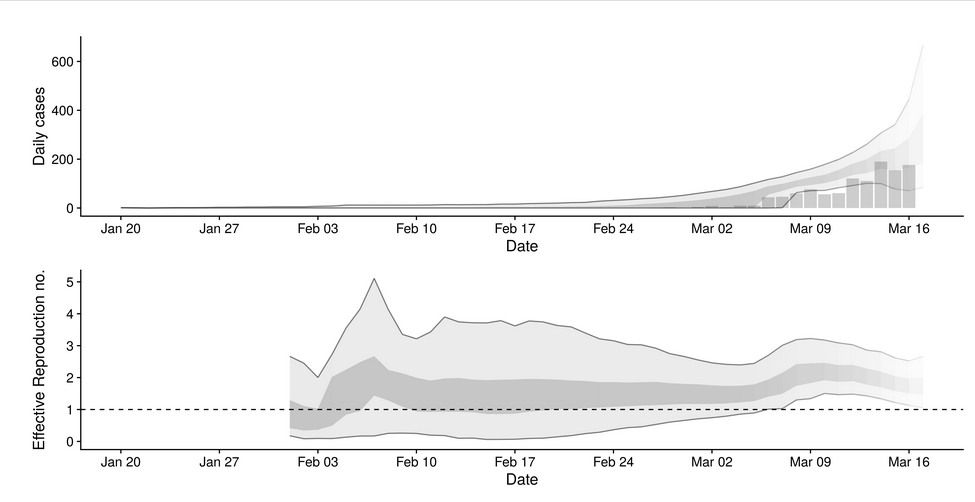
COVID-19 in The Netherlands
These graphs take some processing and are not up to the minute, but they do show the numbers we need to know. Other sites may be more exciting, but I prefer this one!
(In an interesting twist, one of the key people behind this project tested positively for Corona, but he tells us he is only feeling “rough” and is working from home)
Recent interesting papers
Papers (actually non-peer reviewed preprints) that look interesting, but have not been (fully) absorbed into a specific section of this page:
- 8th of March: Clinical presentation and virological assessment of hospitalized cases of coronavirus disease 2019 in a travel-associated transmission cluster by Charite Universitaetsmedizin Berlin, Berlin, Germany. Touches on immune response and viral shedding and criteria for when a patient might no longer be infective. Discussion by the incomperable Kai Kupferschmidt in this twitter thread. Explainer article on statnews.com.
- 10th of March: The demand for inpatient and ICU beds for COVID-19 in the US: lessons from Chinese cities, containing the following absolutely KEY insight, backed up with data: “In Wuhan, strict disease control measures were implemented six weeks after sustained local transmission of SARS-CoV-2. Between January 10 and February 29, COVID-19 patients accounted for an average of 637 ICU patients and 3,454 serious inpatients on each day. During the epidemic peak, 19,425 patients (24.5 per 10,000 adults) were hospitalized, 9,689 (12.2 per 10,000 adults) were considered to be in serious condition, and 2,087 patients (2.6 per 10,000 adults) needed critical care per day. In Guangzhou, strict disease control measures were implemented within one week of case importation. Between January 24 and February 29, COVID-19 accounted for an average of 9 ICU patients and 20 inpatients on each day”
- 14th of March: A human monoclonal 1 antibody blocking SARS-CoV-2 infection. Details how work on SARSv1 helped find a ‘-mab’ that blocks COVID-19.
- 16th of March: Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus argues persuasively that much of the transmission was from “undocumented” patients. This does not mean these patients were symptom-free, but they never got tested.
Twitter must-follows
There is a LOT of noise on twitter about COVID-19. However, here is a list of highly responsible, very high signal-to-noise ratio tweeters:
- @kakape, Kai Kupferschmidt, science journalist. molecular biologist. Contributing Correspondent at Science Magazine
- @mlipsitch, Marc Lipsitch, Infectious disease epidemiologist and microbiologist, Harvard.
- @HelenBranswell, Senior writer, infectious diseases at the excellent Statnews.com.
- @RichardLehman1, the master reviewer of medical journals is back! Richard is someone I wish we had more of - an actual (retired) healthcare professional who is also an academic.
Another outstanding follow is @COVID_Evidence which live-tweets the latest preprints and clinical trials.
Russ Garrett also maintains an exhaustive set of bookmarks.
Todo: other open questions
This content needs to be written. If you have good links or data, bert@hubertnet.nl or @bert_hu_bert are the places to send them.
- Are ‘superspreading events’ important? Maybe. May drive >80% of transmission. This is a good rationale for canceling large events. Technical term is ‘overdispersion’. An anecdote, more detail
- Children get infected readily with COVID-19 but they have very mild disease. But do they spread it effectively? In other words, does closing schools help a lot (directly)? It is known that closing schools binds parents to their houses, which provides an indirect way to limit spread of disease.
- Why is COVID-19 so lethal in Italy? (appears to be lots of infections among very old people, and by now (10th of March) an overwhelmed healthcare system)
- Why is COVID-19 so lethal in The Netherlands? Why does The Netherlands have 200 people in intensive care whereas Austria, with slightly fewer people testing positive, has 17? (20th of March)
- Why is COVID-19 almost non-lethal in Germany? 20th of March update: this FT article notes Germany is doing 160k tests a week, which is more than Korea.
- How can China be reporting only double digit new infections? Has China actually restarted its society? Perhaps not so much. As of March 12th this is becoming somewhat of a bigger mystery since China is now reporting single digit case numbers from Wuhan. 20th of March, or 0 cases now. Hard to believe.