COVID-19: Things We're Not Even Trying
As COVID-19 drags on, I’ve tried to stay optimistic about scientific and medical developments. By highlighting research, I have hoped to explain (in Dutch and English) how various things will work to defeat COVID-19, and how to look out for your health.
But all this time I’ve been frustrated about the things we are not doing, or are not doing enough of.
10th of January 2021 update: The advent of new highly transmissible variants makes this all even worse.
Things that have been tried with great gusto
Remember remdesivir, which was immediately rushed out to testing? After a third party trial it was found remdesivir did not work, and there were good reasons to suspect that already. It still got approved in the US somehow.
The medical field also did hundreds of trials on (hydroxy)chloroquine, popular in some political circles. Sadly, that too did not turn out to work, but it could theoretically have. Although there were too many trials, researching this drug was worth it.
Meanwhile, serious research found out that a common existing drug (dexamethasone) worked pretty well on a subset of very ill patients.
It turns out however that there are many other possible treatments and strategies that aren’t being taken seriously, despite serious evidence. And then there are some pretty harmless things that have accumulated some evidence, but that are studiously being ignored because there is not yet enough evidence.
Why the medical field is so conservative
The remdesivir and (hydroxy)chloroquine trials have left their mark - almost no one is now rushing in to test new things. The medical field is usually pretty conservative, as exhibited by the medical establishment widely advising against facemasks originally (’there is no proof’), or the refusal to even contemplate aerosol transmission. We now know this is an important route of transmission.
The medical field has reasons to be conservative, as it has historically strayed a lot, often while trying rather obvious things. The biggest error that I’m aware of was Dutch, I’m ashamed to say.
Don Poldermans published research that showed that liberally administering beta-blockers before and after major surgery would save lives. This was duly turned into a European guideline that stayed in force for many years. It then turned out that Poldermans had falsified his data, and that the guideline actually increased mortality by 27%. This has been extrapolated to have cost as many as hundreds of thousands of lives (!).
Given this, you can imagine that the medical field is hesitant to try even pretty plausible things. And if you wonder, why did I not ever hear about Don Poldermans, know there are more medical reversals like that. It has been traumatic. The field does not like to talk about it.
Given this, the world of medicine is currently very determined to only accept treatments after massive amounts of evidence, preferably accumulated by trials so large they are out of reach of almost everyone except the largest pharmaceutical companies.
Paradoxically, this may not actually be helping - companies like Gilead have the ability to organize massive trials for their medicines, which then get accepted even if the results are not very promising. It would be far better if academia and institutes ran clinical trials themselves, perhaps smaller ones, but at least under their own full control. This worked very well for dexamethasone for example.
Governments and public health are currently running a few COVID-19 trials. The UK is a massive force for good here, as noted by the ongoing results from the RECOVERY trial. Another institutional trial doing very worthwhile things is REMAP-CAP. We could do with a lot more of this.
Promising things we’re not studying well enough
The COVID-19 situation is not looking good - numbers are heading in the wrong direction in many places. Vaccines appear very promising, but are not there yet in quantity. So we should have a healthy interest in possible treatment and prevention options.
Below I mention three things we should be taking more seriously. To be sure, I’m not claiming all of these things will cure us of COVID-19. But I am claiming that we’re also not taking these candidate measures seriously enough.
Vitamin D
For starters, there is vitamin D. Extremely abbreviated, we know that being vitamin D deficient is associated with very very bad COVID-19 outcomes. In one German study for example, the fraction of COVID-19 deaths was 14 times higher among those deficient in vitamin D - and there are 22 studies showing similar things.
The obvious thing would be to make sure no one is vitamin D deficient during this pandemic. Vitamin D deficiency is very common during winter months. Many governments have standing guidelines for women, older people, people of color and other groups to take vitamin D supplements to prevent deficiencies.
Yet public health professionals and governments are widely not doing anything around vitamin D since “there is no proof it will help”. This includes not reminding people of existing guidelines (!).
When confronted, authorities will say there have been disappointing vitamin D trials in the past for other diseases (like cancer), so we should ignore all this until there is more proof. Meanwhile, serious proof is only being gathered in a few smaller trials, which are then pooh-poohed as being too small, even if the results are spectacular.
It boggles the mind. Meanwhile, please take all the care you can not to be vitamin D deficient this winter. Sadly, being outdoors in winter months does not help, so this comes down to vitamin D3 pills for now. In many cases, all you need to do is follow existing guidelines!
I’ve previously written a huge post “Vitamin D: the New COVID-19 Chloroquine?” that covers the situation in great detail.
Ivermectin
This already widely used drug was mentioned early on in the pandemic, often in the same breath as hydroxychloroquine. A fraudulent paper on chloroquine was published and sadly the same group also provided data for a fraudulent preprint on ivermectin. This was very unhelpful. But this is not ivermectin’s fault of course.
22 studies on ivermectin and COVID-19 have now been performed and all 22 have been positive. Specifically, 100% of the 9 Randomized Controlled Trials (RCTs) report positive effects - and these are the most stringent tests you can do. Many of the most widely used medicines for other diseases can not claim 9 positive RCTs.
Ivmmeta.com hosts a repository of all results and performs a running meta-analysis on them.
Yet in COVID-19 treatment guidelines, you’ll barely hear a peep.
One reason why the medical field is shy about ivermectin is the memory of the original fraudulent preprint, plus that in laboratory experiments, the medicine does work, but only at higher doses than are feasible for treatment. But meanwhile, despite these lab results, 22 trials are positive. “But does it also work in theory?”.
Again, it is immensely frustrating that these promising results are not taken more seriously.
9th of January 2021 UPDATE: It appears the very useful UK RECOVERY trial will evaluate ivermectin.
11th of September 2021 UPDATE: It appears many of the Ivermectin trials were fraudulent or at least bad. If you average out a lot of bad trials, you do not get one good trial.
Antigenic tests
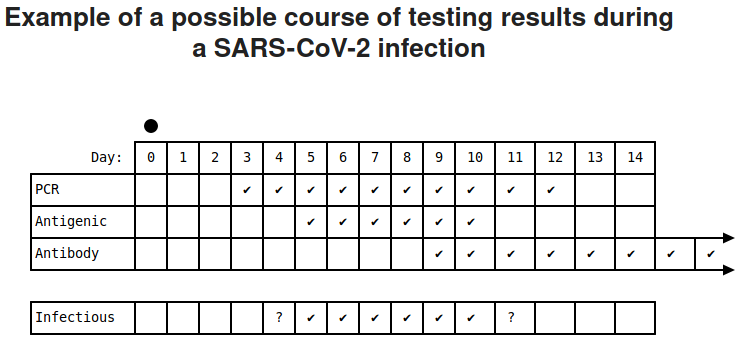
The gold standard for detecting a (past) SARS-CoV-2 infection is the PCR test. This test, if administered well, can detect disease before, during and long after falling ill. It really is very very sensitive (and specific - it only detects SARS-CoV-2). Full marks. The PCR test also takes many hours to run, requires expert lab technicians, advanced machinery and scarce reagents (chemicals).
Antigenic tests can be run at home by anyone who is able to stick a swab up their nose and twist it a few times. The results appear in minutes, no equipment is required. I’ve performed this test on myself and others and it really is very easy. Every test costs 8 euros right now, but I suspect that in bulk it could be a lot cheaper.
The antigenic test detects actual virus particles. The PCR test detects viral genetic material. In several evaluations by some of the best medical institutes around, it has been shown that good antigenic tests detect 95% or more of patients with live virus particles in their noses. This likely translates to 95% of infectious people, although formally we can’t be sure.
PCR tests are able to detect people that don’t yet have (many) live virus particles in their nose. In addition, they also detect people that are far enough along in the disease that they are no longer infectious.
There are two ways to look at the antigenic test. One is to compare it apples to apples to the PCR test, and in that case, it is a somewhat lousy PCR test. Its predictive value is worse and it also doesn’t detect COVID-19 in people who are no longer infectious. Most medical people consider the antigenic test to be a bad PCR test - even though it is not much less sensitive in clinical practice.
If you look at the antigenic test as a way to find people with SARS-CoV-2 in their nose, the antigenic test is way way better than the PCR test. It is faster, cheaper and also far more specific - it finds exactly what you were looking for (virus particles), unlike the PCR test that can stay positive for months by detecting bits of RNA.
Unsurprisingly, a lot of the medical field does not look at antigenic tests this way.
But if you did, you could imagine wonderful things you could be doing with antigenic tests, like for example returning mildly symptomatic people back to work, as long as you test them just before they enter the building.
If there are events that just have to happen in person, you can make them lots safer by testing everyone beforehand. This will screen out over 95% of infectious people from your meeting. Imagine that.
Or let’s say someone tests positive in a school class - you could quickly test the whole class and make sure the right people isolate immediately. Test the rest for a few days more and you’ll be able to stop an outbreak.
Now, a PCR test would be even more sensitive for this use case (pick up more people) - but the thing is, we should not compare the test you can do easily (antigenic) with the test that did not happen (the PCR one).
If antigenic tests were widely available they could be a game changer. Instead, we are hung up with people arguing the PCR test is more sensitive. But that is not the test you could run at the office to improve the safety of your working environment!
Please do note that no test is perfect - nowhere in this post do I argue to do non-essential in person events (like indoor dining). But if you have events that have to happen, you can make them a lot safer with antigenic tests.
Michael Mina of Harvard Medical School explains the situation very well in this Time article.
Now that these tests exist in quantity, what we should be doing is developing a strategy how to deploy them wisely. This involves deciding when such tests should be used and training people how to use them. But nothing like that appears to be happening.
Some other possible treatments
I mentioned vitamin D, ivermectin and antigenic tests, but there are other existing/modified medicines that appear to be promising, if only we had more proof - proof we are not gathering rapidly enough.
- Bromhexine, widely available outside the US to help with coughing, appears to be very successful in at least one trial. There are good theoretical reasons to think bromhexine (sold as Bisolvon in Europe) should be effective. One trial appears to be running.
- Nebulised interferon beta-1a - successful in a small phase 2 study by UK company Synairgen. And like Bromhexine, there are strong theoretical arguments why this should indeed be effective. A single followup trial has been running for months.
Summarising
COVID-19 is still threatening. We should take all promising avenues for relief seriously, including very plausible ones like vitamin D status, ivermectin and developing a responsible rapid testing strategy.
It is highly frustrating that the medical field is not very interested in these things, citing lack of absolute proof, but then also does not do the work on gathering that proof. This with the notable exception of the RECOVERY and REMAP-CAP trials.